Heading out of town? Leaving your troubles behind? Off on an important business trip? Whenever you travel, your diabetes makes the trip with you.
While diabetes shouldn't stop you from traveling in style, you will need to do some careful planning. Here are some helpful diabetes travel tips from the National Diabetes Education Program:
PLAN AHEAD
• Get all your immunizations. Find out what's required for where you're going and make sure you get the right shots on time.
• Control your ABCs. See your healthcare provider for a checkup four to six weeks before your trip to make sure your alcohol, blood pressure and cholesterol are under control and in a healthy range before you leave.
• Ask your healthcare provider for a prescription and a letter explaining your diabetes medication, supplies and any allergies. Carry this with you at all times on your trip. The prescription should be for insulin or diabetes medications and could help in case of an emergency.
• Wear identification that explains you have diabetes. The identification should be written in the languages of the places you are visiting
.• Plan for time zone changes. Make sure you'll always know when to take your diabetes medicine, no matter where you are. Remember: eastward travel means a shorter day. If you inject insulin, less might be needed. Westward travel means a longer day, so more insulin might be needed.
• Find out how long the flight will be and whether meals will be served. However, you should always carry enough food to cover the entire flight time in case of delays or unexpected schedule changes.
PACK PROPERLY
• Take twice the amount of diabetes medication and supplies that you'd normally need. It's better to be safe than sorry.
• Keep your insulin cool by packing it in an insulated bag with refrigerated gel packs.
• If you use insulin, make sure you also pack a glucagon emergency kit.
• Make sure you keep your medical insurance card and emergency phone numbers handy.
• Don't forget to pack a first-aid kit with all the essentials.
WHEN FLYING
• Plan to carry all your diabetes supplies in your carry-on luggage. Don't risk a lost suitcase.
• Have all syringes and insulin delivery systems (including vials of insulin) clearly marked with the pharmaceutical preprinted label that identifies the medications. The FAA recommends that patients travel with their original pharmacy labeled packaging.
• Keep your diabetes medications and emergency snacks with you at your seat. Don't store them in an overhead bin.
• If the airline offers a meal for your flight, call ahead for a diabetic, low-fat or low-cholesterol meal.
• Wait until your food is about to be served before you take your insulin. Otherwise, a delay in the meal could lead to low blood glucose.
• If no food is offered on your flight, bring a meal on board yourself.
• If you plan on using the restroom for insulin injections, ask for an aisle seat for easier access.
• Don't be shy about telling the flight attendant that you have diabetes, especially if you are traveling alone.
• When drawing up your dose of insulin, don't inject air into the bottle. The air on your plane will probably be pressurized.
• Because prescription laws can be very different in other countries, write for a list of International Diabetes Federation groups: IDF, 1 Reu de Faeqz, B-1000, Belgium, or visit www.idf.org. Get a list of English-speaking foreign doctors in case of an emergency. Contact the American Consulate, American Express or local medical schools for a list of doctors.
• Insulin in foreign countries comes in different strengths. If you purchase insulin in a foreign country, be sure to use the right syringe for the strength. An incorrect syringe might cause you to take too much or too little insulin.ON THE ROAD
• Don't leave your medications in the trunk, glove compartment or near a window, where they might overheat. If possible, carry a cooler in the car to keep medications cool.
• Bring extra food with you in the car in case you can't find a restaurant.
GENERAL TRAVELING TIPS
• Stay comfortable and reduce your risk for blood clots by moving around every hour or two.
• Always tell at least one person traveling with you about your diabetes.
• Protect your feet. Never go barefoot in the shower or pool.
• Check your blood glucose often. Changes in diet, activity and time zones can affect your blood glucose in unexpected ways.You might not be able to leave your diabetes behind, but you can control it and have a relaxing, safe trip.
To learn more about controlling your diabetes, visit the National Diabetes Education Program at www.ndep.nih.gov.
"TRAVEL HEALTH
Diabetes doesn't have to ruin your vacation plans
By DR. LARRY G. BARATTA For travelers with chronic health problems such as diabetes, managing the condition has its challenges.
But with proactive planning, someone with diabetes can have a safe and enjoyable trip. Before a trip, consult your physician to weigh the risks of traveling to developing countries, particularly if you have complications such as foot ulcers, diabetic heart, eye or kidney disease.
BEFORE YOU TRAVEL
• Medical records: Take a letter from your physician attesting to your diabetes diagnosis, listing your medications, including syringes, if applicable. Also, take a copy of your most recent medical records and laboratory reports.
If you need to consult with a foreign doctor, this information will be most useful. Compile a list of physicians in the cities you are traveling to. The International Association for Medical Assistance of Travelers (716-754-4883; http://www.iamat.org/) and the International Diabetes Federation (011-32-2-538-5511; http://www.idf.org/) are two useful resources.
• Medication list: Print a copy of your current medications, including the dosages. This list should also include other medications you take. Take extra supplies (oral or insulin) with you in the event there are travel delays or trip interruptions.
Over-the-counter medicines including anti-diarrheal and anti-nausea medication are also important.
Pack a fever thermometer.
• Medication labeling: Make sure your medication is labeled properly (original containers are preferred) and that it is stored in zip-lock bags, especially for liquids.
• Medication storage: If you need insulin, there are many travel kits that are compact and will help protect your supplies: insulin vials, syringes, alcohol preps, etc. Insulin does not have to be refrigerated. But storing it in extreme temperatures may affect its strength.
• Diabetes management supplies: Take extra blood and urine testing supplies. Make sure your blood glucose monitor works properly, is cleaned and calibrated and you have an extra set of batteries. Take extra syringes. Insulin syringes in North America have different measurement markings on the barrel than those sold overseas.
If you run out of insulin and need to purchase it overseas, you will also need to buy syringes.
Pack enough snack foods like crackers, peanut butter, cheese and juice. Also pack hard candy to treat low blood sugar.
Properly tag your supply bags with your contact information.
A diabetes ID bracelet and wallet diabetes identification card are essential.
Bring a compact medical sharps container to dispose of used syringes.
• Additional resources: Consider getting travel medical insurance. This should cover complete medical care, including hospitalization, air ambulance and emergency medical evacuation. Travel insurance plans are available through companies including MultiNationalUnderwriters, Specialty Risk International and Travelex.
AT THE AIRPORT
• Recent Transportation Security Administration restrictions have caused difficulty for diabetic travelers. Visit http://www.tsa.gov/ (or call 866-289-9673) for more information.
• Notify the TSA screener that you have diabetes and are carrying supplies. If you wear a nonremovable insulin pump, be sure to alert them, as well.
• You may request a visual inspection of your supplies instead of X-raying them.
DURING YOUR FLIGHT
Request an onboard diabetic meal. Bring plenty of ''diabetic friendly'' snacks.
Take your insulin just before your meal is served.
Cabin pressure is lower than the pressure in the insulin bottle. In order to help equalize the pressure, insert the syringe (without the plunger) into the vial. Be careful not to inject air into the vial.
Stay well hydrated by drinking plenty of fluids. Cabin air is dry and low in humidity. Seasoned air travelers use saline nasal spray periodically during the flight to keep the nasal passages moist.
Exercise during long-haul flights to increase circulation, particularly in the legs. This will help prevent formation of blood clots. Wearing support hosiery also helps.
AFTER YOU ARRIVE
Pace yourself. After a long-haul flight, your body needs to adjust.
Check your blood sugar level often. That's why you need to pack extra test strips.
Plan sightseeing excursions around taking your insulin and meals. A very active schedule may result in lower blood glucose.
Take snacks and food on sightseeing trips in case food is not available at your destination.
Be careful what you consume. Water and ice cubes can cause gastrointestinal ailments. Ice cubes may contain bacteria responsible for causing diarrhea. Drink bottled water and avoid other sources.
Wear comfortable shoes and socks. This will reduce developing sores or blisters on your feet. Check your feet daily for redness, swelling and scratches. Don't break in a new pair of shoes during the trip."
Dr. Larry G. Baratta chief medical officer of Passport Health serving South Florida.
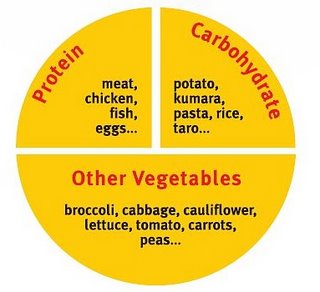
Eat healthy and live longer.